General Advisory for H1N1 (FLU)2012
On 10th August, 2010, Director-General Health Services & WHO announced that the H1N1 Influenza pandemic has moved into the post-pandemic period and it ceases to be a public health emergency of international concern (in accordance with International Health Regulations 2005). However, WHO mentioned that localized outbreaks of various magnitudes are likely to continue.
Recently in the month of March, 2012 few cases of h1n1 have resurged all over India including Delhi. To control the further spread of the disease abundant precautions are needed and the mechanism has to re-galvanized. The effective and proven preventive guidelines are issued for general public at large.
For Travellers:
1. Before leaving for India ascertain your vaccination status. Keep vaccination record, if already vaccinated. Vaccination with H1N1 vaccine is not mandatory.
2.During Travel if suffering from fever, cough, running nose, sore throat and difficulty in breathing while on flight, ask for the triple layer face mask, cover your face with it and contact on arrival, the Help Desk at the Delhi International Airport for assistance. Each National & international flight should have the provision of triple layer surgical mask.
3.During period of stay in India (for Foreigners)
Look for Symptoms of Influenza A H1N1 (swine flu):
Visitors should be familiar with the symptoms of this disease, namely fever, cough, running nose, sore throat and difficulty in breathing. They should contact the Govt./Pvt. Hospitals identified for h1n1 management. One can see the list of such hospitals on website www.mohfw.nic.in
If you think you have symptoms of Flu (For foreigners):
- Contact the medical officer posted at H1N1 screening centre (24x7) in the nearest hospital.
- As per advice of the Nodal Officer (H1N1) or medical doctor if you have to stay at home/hotel room (Home Quarantine), use triple layer surgical mask (which would be provided by the Medical unit) and take complete treatment. Avoid close contact with others for 7 days (after your symptoms begin) or until you have been symptom-free for 24 hours whichever is longer.
- Observe following Dos & Don’ts during illness period.
- Report to nearest identified health facility if symptoms aggravate (high fever, difficulty in breathing, blue coloration of the skin or lips, blood in sputum).
- Anyone who contracts H1N1 during the stay in India will be given access, free consultation, diagnosis and treatment in Govt./Pvt. health facilities notified by the Government.
Follow simple public health measures to prevent spread of H1N1 Flu (Do’s and Dont’s)
DOs:
- Cover your mouth and nose with a handkerchief or tissue when you cough or sneeze.
- Wash your hands often with soap and water or use an alcohol based hand gel.
- Avoid touching your eyes, nose or mouth.
- Avoid visiting crowded places.
- Stay more than an arm's length from persons afflicted with h1n1.
- Take adequate rest, get plenty of sleep, water and eat nutritious food.
- Disinfect the handkerchief and destroy the used tissue properly.
DO NOTs:
- Shake hands or hug in greeting.
- Take medicines without consulting a physician.
- Meet relatives and friends.
4. After reaching back
- Continue to monitor your health for 10 days.
- Report to nearest health facility if you develop symptoms of flu.
For More Information
- Visit http://www.mohfw-h1n1.nic.in
- Contact National Help Line -011-23921401
Ministry of Health & Family Welfare
Pandemic Influenza A (H1N1)
Guidelines on categorization of Influenza A H1N1 cases during screening for home isolation, testing treatment, and hospitalization (Revised on 05.10.09)
In order to prevent and contain outbreak of Influenza-A H1N1 virus for screening, testing and isolation following guidelines are to be followed:
At first all individuals seeking consultations for flu like symptoms should be screened at healthcare facilities both Government and private or examined by a doctor and these will be categorized as under:
Category- A
- Patients with mild fever plus cough / sore throat with or without bodyache, headache, diarrhoea and vomiting will be categorized as Category-A. They do not require Oseltamivir and should be treated for the symptoms mentioned above. The patients should be monitored for their progress and reassessed at 24 to 48 hours by the doctor.
- No testing of the patient for H1N1 is required.
- Patients should confine themselves at home and avoid mixing up with public and high risk members in the family.
Category-B
1. In addition to all the signs and symptoms mentioned under Category-A, if the patient has high grade fever and severe sore throat, may require home isolation and Oseltamivir;
2. In addition to all the signs and symptoms mentioned under Category-A, individuals having one or more of the following high risk conditions shall be treated with Oseltamivir:
- Children with mild illness but with predisposing risk factors.
- Pregnant women;
- Persons aged 65 years or older;
- Patients with lung diseases, heart disease, liver disease, kidney disease,blood disorders, diabetes, neurological disorders, cancer and HIV/AIDS;
- Patients on long term cortisone therapy.
- No tests for H1N1 is required for Category-B (1) and (2).
- All patients of Category-B (i) and (ii) should confine themselves at home and avoid mixing with public and high risk members in the family.
Category-C
In addition to the above signs and symptoms of Category-A and B, if the patient has one or more of the following:
- Breathlessness, chest pain, drowsiness, fall in blood pressure, sputum mixed with blood, bluish discoloration of nails;
- Children with influenza like illness who had a severe disease as manifested by the red flag signs (Somnolence, high and persistent fever, inability to feed well, convulsions, shortness of breath, difficulty in breathing, etc).
- worsening of underlying chronic conditions.
All these patients mentioned above in Category-C require testing, immediate hospitalization and treatment.
Fundamental principles of isolation are
- Standard precautions
- Droplet precautions
- Airborne precautions and
- Contact precautions.
An isolation facility needs to follow these precautions to ensure that the hospital is not a source of infection to the hospital patients with in and the community. A brief note on each of these precautions is at Annexure-I.
All hospitals indented to screen and admit patients with influenza H1N1 should conform to these guidelines. Identified hospitals would have a separate screening area to screen outdoor patients and an isolation facility to admit those requiring indoor treatment. For clarity, these guidelines are in six parts:
- Generic Guidelines
- Guidelines for pre hospital care
- Guidelines for the screening centre
- Guidelines for isolation facility and
- Guidelines for critical care
- Mortuary care.
(i) Generic guidance
Standard Precautions to be followed at all patient care areas: hand hygiene, Gloves and use of personal protective equipment (PPE) to avoid direct contact with patient's blood, body fluids, secretions and non-intact skin, prevention of needle stick/sharp injury and cleaning and disinfection of the environment and equipment.
Droplet precautions to be followed when caring for patients with influenza A H1N1 (masks, respirators and eye shield) in isolation facilities.
Airborne and Contact Precautions should complement Standard Precautions while managing case of Pandemic influenza A H1N1 in critical care facilities. Hospitals should be following the hospital waste management protocols as per the hospital waste management rules.
Dead body should be handled using full cover of PPE.
(ii) Guidelines for Pre Hospital Care
- All identified hospitals to have advanced life support ambulance for have tie up with CATS for immediate transportation of such patient.
- Designated paramedic and driver for the ambulance
- The ambulance staff should follow standard precautions while handling the patient and airborne precautions if aerosol generating procedures are done.
- Triple layer surgical masks should be available and worn during transport
- As far as possible the movements should be restricted.
- During transport, optimize the vehicle’s ventilation to increase the volume of air exchange (e.g. opening the windows). When possible, use vehicles that have separate driver and patient compartments.
- Aerosol generating procedures to be avoided to the extent possible.
- Disinfect the ambulance after shifting patient.
- Notify the receiving facility as soon as possible before arrival of the patient.
(iii) Guidelines for setting up Screening Centre
- Purpose of the Screening Centre is to:
- attend to patients of influenza like illness in a separate area as to avoid these
- Patients further infecting other patients of In/Out Patient Department.
- facilitate implementing standard and droplet precautions
- triage the patients
- collect samples.
The screening area would have:
- Adequate waiting space ( about 2000 sq feet) to accommodate 50-100 patients
- preferably stand alone building with separate entry.
- well ventilated to ensure frequent air changes. If air-conditioned, then independent from central air conditioning. Exhaust air to be filtered through HEPA filter (desirable).
- patient’s seating to have at least one meter clearance on all sides. Avoid overcrowding of patients.
- cabins for registration, clinical examination chambers, sample collection rooms and drug distribution centre.
- waiting area adequately cleaned and disinfected.
- source control (e.g. use of tissues, handkerchiefs, piece of cloth or triple layer surgical masks to cover nose and mouth) of the patient in the waiting room when coughing or sneezing, and hand hygiene after contact with respiratory secretions.
- Facility for hand wash. / Wash rooms etc
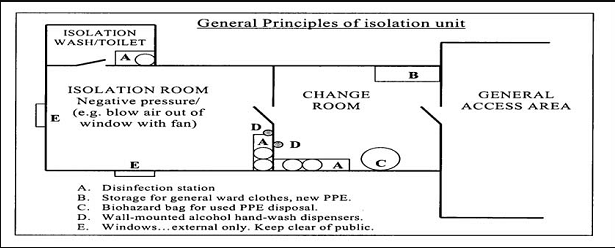
(iv) Guidelines for setting up isolation facility/ward
- Patients should be housed in single rooms, whenever possible.
- However, if sufficient single rooms are not available, beds could be put with a spatial separation of at least 1 m (3 feet) from one another.
- To create a 10 bed facility, a minimum space of 2000 sq feet area is required clearly segregated from other patient-care areas.
- There should be double door entry with changing room and nursing station. Enough PPE should be available in the changing room with waste disposal bins to collect used PPEs.
- Place a puncture-proof container for sharps disposal inside the isolation room/area.
- Keep the patient’s personal belongings to a minimum. Keep water pitchers and cups, tissue wipes, and all items necessary for attending to personal hygiene within the patient’s reach.
- Non-critical patient-care equipment (e.g. stethoscope, thermometer, blood pressure cuff, and sphygmomanometer) should be dedicated to the patient, if possible. Any patient-care equipment that is required for use by other patients should be thoroughly cleaned and disinfected before use.
- Dedicated hand washes and wash room facilities.
- If room is air-conditioned, ensure 12 air changes/hour and filtering of exhaust air. A negative pressure in isolation rooms is desirable for patients requiring aerosolization procedures (intubation, suction nebulisation). These rooms may have stand-alone air-conditioning. These areas should not be a part of the central air-conditioning.
- If air-conditioning is not available negative pressure could also be created through putting up 3-4 exhaust fans driving air out of the room.
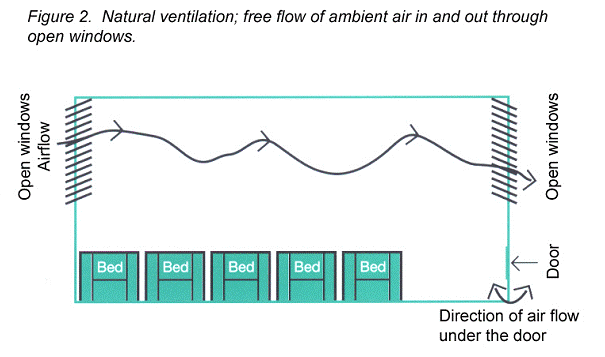
- In District hospital, where there is sufficient space, natural ventilation may be followed. Such isolation facility should have large windows on opposite walls of the room allowing a natural unidirectional flow and air changes. The principle of natural ventilation is to allow and enhance the flow of outdoor air by natural forces such as wind and thermal buoyancy forces from one opening to another to achieve the desirable air change per hour.
- Avoid sharing of equipment, but if unavoidable, ensure that reusable equipment is appropriately disinfected between patients.
- Ensure regular cleaning and proper disinfection of common areas, and adequate hand hygiene by patients, visitors and care givers.
- Visitors to the isolation facility should be restricted. For unavoidable entries, they should use PPE according to the hospital guidance, and should be instructed on its proper use and in hand hygiene practices prior to entry into the isolation room/area.
- Doctors, nurses and paramedics posted to isolation facility need to be dedicated and not to be allowed to work in other patient-care areas.
- Consider having designated portable X-ray equipment
- Corridors with frequent patient transport should be well-ventilated.
- All health staff involved in patient care should be well trained in the use of PPE.
- A telephone or other method of communication should be set up in the isolation room/area to enable patients or family members/visitors to communicate with nurses.
(V) Guidelines for Critical Care facility
- At least one identified hospital may have a 10 bedded dedicated intensive care facility at State Capital.
- The critical care facility requires to follow all the guidelines as mentioned above for infection control.
- Also have arrangement equal to 12 air changes and maintain negative pressure of 40 psi.
- Should have dedicated equipments. It should also have additional equipments to ventilate at least 10 patients manually.
- A telephone or other method of communication should be set up in the isolation room/area to enable patients or family members/visitors to communicate with nurses inside the facility.
- Would have an information board outside to update relatives on the clinical status.
(vi) Mortuary care
- Mortuary staff should apply Standard Precautions i.e. perform proper hand hygiene and use appropriate PPE (use of gown, gloves, facial protection if there is a risk of splashes from patient's body Fluids/ secretions onto staff's body and face).
- Embalming, if required should be conducted according to usual procedures, subject to local regulations/legislation.
- Hygienic preparation of the deceased (e.g. cleaning of body, tidying of hair, etc) also may be done using standard precautions.
Annexure-I
Fundamentals of Isolation Precautions
1. Standard Precautions-
Use Standard Precautions, or the equivalent, for the care of all patients. The standard precautions are:
1.1 Hand washing
Wash hands after touching blood, body fluids, secretions, excretions, and contaminated items, whether or not gloves are worn. Wash hands immediately after gloves are removed, between patient contacts, and when otherwise indicated to avoid transfer of microorganisms to other patients or environments. It may be necessary to wash hands between tasks and procedures on the same patient to prevent cross-contamination of different body sites.
1.2 Gloves
Wear gloves (clean, non sterile gloves are adequate) when touching blood, body fluids, secretions, excretions, and contaminated items. Put on clean gloves just before touching mucous membranes and non- intact skin. Change gloves between tasks and procedures on the same patient after contact with material that may contain a high concentration of microorganisms. Remove gloves promptly after use, before touching non contaminated items and environmental surfaces, and before going to another patient, wash hands immediately to avoid transfer of microorganisms to other patients or environments.
1.3 Mask, Eye Protection, Face Shield
Wear a mask and eye protection or a face shield to protect mucous membranes of the eyes, nose, and mouth during procedures and patient-care activities that are likely to generate splashes or sprays of blood, body fluids, secretions, and excretions.
1.4 Gown
Wear a gown (a clean, non sterile gown is adequate) to protect skin and to prevent soiling of clothing during procedures and patient-care activities that are likely to generate splashes or sprays of blood, body fluids, secretions, or excretions. Select a gown that is appropriate for the activity and amount of fluid likely to be encountered. Remove a soiled gown as promptly as possible and wash hands to avoid transfer of microorganisms to other patients or environments.
1.5 Patient- Care Equipment
Handle used patient-care equipment soiled with blood, body fluids, secretions, and excretions in a manner that prevents skin and mucous membrane exposures, contamination of clothing, and transfer of microorganisms to other patients and environments. Ensure that reusable equipment is not used for the care of another patient until it has been cleaned and reprocessed appropriately. Ensure that single-use items are discarded properly.
1.6 Environmental Control
Ensure that the hospital has adequate procedures for the routine care, cleaning, and disinfection of environmental surfaces, beds, bed rails, bedside equipment, and other frequently touched surfaces and ensure that these procedures are being followed.
1.7 Linen
Handle, transport, and process used linen soiled with blood, body fluids, secretions, and excretions in a manner that prevents skin and mucous membrane exposures and contamination of clothing and that avoids transfer of microorganisms to other patients and environments.
1.8 Occupational Health and Blood borne Pathogens
Take care to prevent injuries when using needles, scalpels, and other sharp instruments or devices; when handling sharp instruments after procedures; when cleaning used instruments; and when disposing of used needles. Never recap used needles, or otherwise manipulate them using both hands, or use any other technique that involves directing the point of a needle toward any part of the body; rather, use either a one-handed "scoop" technique or a mechanical device designed for holding the needle sheath. Do not remove used needles from disposable syringes by hand, and do not bend, break, or otherwise manipulate used needles by hand. Place used disposable syringes and needles, scalpel blades, and other sharp items in appropriate puncture-resistant containers, which are located as close as possible to the area in which the items were used, and place reusable syringes and needles in a puncture-resistant container for transport to the reprocessing area. Use mouthpieces, resuscitation bags, or other ventilation devices as an alternative to mouth-to-mouth resuscitation methods in areas where the need for resuscitation is predictable.
1.9 Patient Placement
Place a patient who contaminates the environment or who does not (or cannot be expected to) assist in maintaining appropriate hygiene or environmental control in a private room. If a private room is not available, consult with infection control professionals regarding patient placement or other alternatives.
2. Airborne Precautions
In addition to Standard Precautions, use Airborne Precautions, or the equivalent, for patients known or suspected to be infected with microorganisms transmitted by airborne droplet nuclei (small-particle residue {5µm or smaller in size} of evaporated droplets containing microorganisms that remain suspended in the air and that can be dispersed widely by air currents within a room or over a long distance).
2.1 Patient Placement.
Place the patient in a private room that has
- monitored negative air pressure in relation to the surrounding area,
- 12 air changes per hour, and
- appropriate discharge of air outdoors or monitored high-efficiency filtration of room air before the air is circulated to other areas in the hospital. Keep the room door closed and the patient in the room. When a private room is not available, place the patient in a room with a patient who has active infection with the same microorganism, unless otherwise recommended, but with no other infection. When a private room is not available and cohorting is not desirable, consultation with infection control professionals is advised before patient placement.
2.2 Respiratory Protection
Wear respiratory protection (three layered surgical mask/N 95 respirator) when entering the room of a patient.
2.3 Patient Transport
Limit the movement and transport of the patient from the room to essential purposes only. If transport or movement is necessary, minimize patient dispersal of droplet nuclei by placing a surgical mask on the patient, if possible.
3. Droplet Precautions
In addition to Standard Precautions, use droplet precautions, or the equivalent for a patient known or suspected to be infected with microorganisms transmitted by droplets (large-particle droplets {larger than 5 µm in size} that can be generated by the patient during coughing, sneezing, talking, or the performance of procedures).
3.1 Patient Placement
Place the patient in a private room. When a private room is not available, place the patient in a room with a patient(s) who has active infection with the same microorganism but with no other infection (cohorting). When a private room is not available and cohorting is not achievable, maintain spatial separation of at least 3 ft between the infected patient and other patients and visitors. Special air handling and ventilation are not necessary, and the door may remain open.
3.2 Mask
In addition to standard precautions, wear a mask when working within 3 ft of the patient. (Logistically, some hospitals may want to implement the wearing of a mask to enter the room.)
3.3 Patient Transport
Limit the movement and transport of the patient from the room to essential purposes only. If transport or movement is necessary, minimize patient dispersal of droplets by masking the patient, if possible.
4. Contact Precautions
In addition to Standard Precautions, use Contact Precautions, or the equivalent, for specified patients known or suspected to be infected or colonized with epidemiologically important microorganisms that can be transmitted by direct contact with the patient (hand or skin-to-skin contact that occurs when performing patient-care activities that require touching the patient's dry skin) or indirect contact (touching) with environmental surfaces or patient-care items in the patient's environment.
4.1 Patient Placement
Place the patient in a private room. When a private room is not available, place the patient in a room with a patient(s), who has active infection with the same microorganism but with no other infection (cohorting).
4.2 Gloves and Hand Washing
In addition to wearing gloves as outlined under Standard Precautions, wear gloves (clean, non-sterile gloves are adequate) when entering the room. During the course of providing care for a patient, change gloves after having contact with infective material that may contain high concentrations of microorganisms (fecal material and wound drainage). Remove gloves before leaving the patient's environment and wash hands immediately with an antimicrobial agent or a waterless antiseptic agent. After glove removal and hand-washing, ensure that hands do not touch potentially contaminated environmental surfaces or items in the patient's room to avoid transfer of microorganisms to other patients or environments.
4.3 Gown
In addition to wearing a gown as outlined under Standard Precautions, wear a gown (a clean, non-sterile gown is adequate) when entering the room if you anticipate that your clothing will have substantial contact with the patient, environmental surfaces, or items in the patient's room.
4.4 Patient Transport
Limit the movement and transport of the patient from the room to essential purposes only. If the patient is transported out of the room, ensure that precautions are maintained to minimize the risk of transmission of microorganisms to other patients and contamination of environmental surfaces or equipment.
4.5 Patients-Care Equipment
When possible, dedicate the use of non critical patient-care equipment to a single patient (or cohort of patients infected or colonized with the pathogen requiring precautions) to avoid sharing between patients. If use of common equipment or items is unavoidable, then adequately clean and disinfect them before use for another patient.


 स्वास्थ्य सेवा महानिदेशालय
स्वास्थ्य सेवा महानिदेशालय 


