National Leprosy Eradication Programme – Delhi
WHAT IS LEPROSY?
Leprosy/Hansen’s disease is an infectious disease that causes severe, disfiguring skin sores and nerve damage in the arms, legs, and skin areas around the body. The incubation period is 3 to 5 years / till 20 years. Leprosy is caused by mycobacterium lapre it is not so contagious but if one come into close and repeated contact with nose and mouth droplets from someone with untreated leprosy.
Children are more likely to get leprosy than adults. It primarily affects the skin and nerves outside the brain and spinal cords (peripheral Nerves). Eyes and the thin tissue lining the inside the nose. Loss of sensation occur on the affected area of skin with muscle weakness.
What are types of Leprosy?
Leprosy is characterized according to the number and type of skin sores you have. Specific symptoms and your treatment depend on the type of leprosy you have. The types are:
- Paucibacillary/tuberculoid. A mild, less severe form of leprosy. People with this type have only one or a few patches of flat, pale-coloured skin (paucibacillary leprosy). The affected area of skin may feel numb because of nerve damage underneath. Tuberculoid leprosy is less contagious than other forms.
- Multibacillary/lepromatous. A more severe form of the disease. It involves widespread skin bumps and rashes (multibacillary leprosy), numbness and muscle weakness. The nose, kidneys and male reproductive organs may also be affected. It is more contagious than tuberculoid leprosy.
- Borderline. People with this type of leprosy have symptoms of both the tuberculoid and lepromatous forms
| S. No. | Characteristic | PB (Pauci bacillary) | MB (Multi bacillary) |
|---|---|---|---|
| 1. | Skin lesions | 1 – 5 lesions | 6 and above |
| 2. | Peripheral nerve involvement | No nerve / only one nerve with or without 1 to 5 lesions | More than one nerve irrespective of number of skin lesions |
| 3. | Skin smear | Negative at all sites | Positive at any site |
How do you diagnose?
If patients have a suspicious skin sore, your doctor will remove a small sample of the abnormal skin and send it to a laboratory to be examined. This is called a skin biopsy. A skin smear test may also be done. With paucibacillary leprosy, no bacteria will be detected. In contrast, bacteria are expected to be found on a skin smear test from a person with multibacillary leprosy.
What is treatment of Leprosy?
Leprosy can be cured. In the last two decades, more than 14 million people with leprosy have been cured. Treatment depends on the type of leprosy that patients have. The drugs used are dapsone, rifampicin and clofazimine - different combinations of these drugs are recommended depending on whether a person has paucibacillary or multibacillary leprosy. Public Health England (PHE) reports that since the introduction of multi-drug therapy (MDT) in 1982, the number of leprosy cases has been dramatically reduced.Before the introduction of MDT, many leprosy patients could expect to take medicine for life. MDT has been made available free to all leprosy patients in the world by the World Health Organisation.
- Rifampicin: 10 mg/ kg body weight, monthly once
- Clofazimine: 1 mg /kg body weight daily and 6 mg/kg body weight, monthly once
- Dapsone: 2 mg /kg body weight daily.
Duration of treatment: Leprosy persons with PB leprosy need 6 months treatment that must be completed in maximum of 9 consecutive months. This means PB leprosy person cannot miss a total of more than 3 pulses during treatment. MB leprosy person needs 12 months treatment that must be completed in 18 consecutive months. All the efforts must be made to complete 6 pulses in 6 months for PB cases and 12 pulses in 12 months for MB cases. Note: Rarely, specialists may consider treating a person with high bacterial index for more than 12 months; decision is based on clinical and bacteriological evidence.
| Type of leprosyh | Drugs usedh | Frequency of Administration Adults (children in bracket) | Dosage (adult) 15 years above | Dosage (Children 10-14 years)# | Dosage Children Below 10 years* | Criteria for RFT |
|---|---|---|---|---|---|---|
| MB leprosy | Rifampicin | Once monthly | 600 mg | 450mg | 300mg | Completion of 12 monthly pulses in 18 Consecutive months |
| Clofazimine | monthly | 300 mg | 150 mg | 100mg | ||
| Dapsone | Daily Once | 100 mg | 50 mg | 25mg | ||
| Clofazimine | Daily for adults (every other day for children) | 50 mg | 50mg (alternate day, not daily) | 50mg (weekly twice) | ||
| PB leprosy | Rifampicin | Once monthly | 600 mg | 450 mg | 300mg | |
| Dapsone | Daily | 100 mg | 50 mg | 25mg daily or 50 mg alternate day | Completion of 6 monthly pulses 9 consecutive months |
Advantages of Multi Drug Therapy (MDT)
- MDT kills bacilli (M. leprae) in the body. It stops the progress of the disease, prevents further complications and reduces chances of relapse.
- As the M. leprae are killed, the patient becomes non-infectious and thus the spread of infection in the body is reduced. Moreover, chances for transmission of infection to other persons are also reduced to a considerable extent.
- Using a combination of two or three drugs instead of one drug ensures effective cure and reduces chances of development of resistance to the drugs.
- Treatment with multi-drug therapy reduces duration of the treatment.
- Duration of treatment is short and fixed.
- MDT is safe, has minimal side effects and has increased patient compliance.
- Available in blister pack; easy to dispense, store and take.
Indications for prescribing MDT
New case of leprosy: Person with signs of leprosy who have never received treatment before. Other cases: Under NLEP all previously treated cases, who need further treatment are recorded as “other cases”. It has been decided that all migrant cases from another state reporting at any state Health Institution will also be grouped under this category. Other cases include both PB & MB cases.
Cases from outside the state & Temporary migration or cross border cases.
Before deciding a case to be recorded as from other state, the residential status at the place of diagnosis is carefully examined. A person who has migrated and is residing for more than six months, is likely to stay till completion of treatment, and recorded as indigenous case and will not be categorized under “other cases”. Information regarding other cases is shown separately in the monthly progress reports. Once it has been decided that a person needs treatment, register the person in Leprosy Treatment register and make the Leprosy Record Card. Take care to indicate type of patient (new/others) correctly. Decide the regimen and counsel the person
Assessing fitness of a leprosy
Patient for MDT before starting treatment, you must look for the following: Jaundice: If the patient is jaundiced, wait till jaundice subsides. Anemia: If the patient is anaemic, start treatment for anaemia simultaneously along with MDT. Tuberculosis: If the patient is taking Rifampicin, ensure that he continues to take Rifampicin in the dose required for the treatment of tuberculosis along with other drugs in the regimen required for the treatment of leprosy. Allergy to sulpha drugs: If the patient is known to be allergic to sulpha drugs, avoid Dapsone. Refer person for prescription of alternate drug regimen.
Assigning appropriate MDT regimen Based on the grouping, the patients may be given any one of the standard MDT regimen mentioned below. In children, the dose must be adjusted suitably. When the patient has completed the required number of doses the treatment is stopped and RFT (Released from Treatment) is written against the name of the person in the leprosy treatment register.
Treatment of leprosy during pregnancy Why to treat?
MDT is safe and can be continued during pregnancy.
Treatment of leprosy & tuberculosis:
MDT is continued but rifampicin is omitted from MDT for leprosy and is given in the doses recommended as per guidelines of RNTCP.
Treatment of leprosy in HIV positive patients
MDT for leprosy can be safely given to HIV affected persons and to those on antiretroviral therapy.
Side effects of anti-leprosy drugs and its management
- Anaemia
- Abdominal symptoms
- Severe skin complication (Exfoliate dermatitis) Sulphone hypersensitivity, Haemolytic anaemia
- Liver damage (Hepatitis)
- Kidney damage (Nephritis)
Dapsone:
Dapsone may cause haemolysis of red blood cells. People with glucose-6- phosphatase dehydrogenase deficiency are more susceptible to haemolysis. It is usually mild and symptom less. Methaemoglobinaemia may also occur due to dapsone therapy. Lips and nails may develop blue hue that may disappear spontaneously or on reducing the dose and is not an indication to interrupt therapy. Both are rare in therapeutic doses used for leprosy.
Rifampicin
Red discoloration of body fluids
- Flu like illness
- Abdominal symptoms
- Hepatitis (liver damage)
- Allergy
Ensuring regularity of treatment:
- Counsel the person adequately regarding the disease, its curability, duration of treatment and importance of regular & complete treatment. Encourage the person constantly to complete the treatment.
- Tell the basic facts about the disease e.g. disease is curable, skin patches may not disappear or take some time to disappear after the completion of the treatment
- Explain the method of taking drug. Ask person to swallow first dose in front of the health worker / doctor (Assign a person to observe intake of first dose)
- Tell them that medicine is to be collected every 28 days (better to collect 1-2 days in advance).
- Tell the person about possible side effects and when to report.
- Encourage person to ask questions
- Ask person to bring the previous blister pack Every time patient comes to collect medicine, examine and assess for any complication or worsening of disability Contact the person who has not reported to collect the monthly blister pack with the help of your team members or members of the community. Find out the reason and try to find a solution to the patient’s problem. Reasons for interruption of treatment may be many like:
- Poor accessibility of the clinic (Distance/ connectivity / timings)
- Difficulty in taking time off work
- Lack of understanding about disease and importance of regular treatment
- Stigma often fed by negative attitude and fear in the community
- A poor relationship with health care providers Adopt, accompanied MDT, whenever it is essential Ensure timely release from treatment of MDT
Encourage regular and complete treatment
Patients who are not collecting drug on time should be contacted immediately to identify the reasons and take corrective actions. ? Flexibility in MDT delivery (more than one pulse at a time) may be adapted whenever it is essential.
Follow up of patient on MDT
Whenever a patient comes to the PHC, reassure the patient, ensure regularity of treatment, and look for side effects of MDT or sign /symptoms of reaction/ Neuritis.
Completion of treatment with MDT :
Skin lesions due to leprosy may not disappear immediately on completion of fixed duration treatment with MDT. In some people, light-colored patches remain on the skin permanently. Persons with residual patches at the time of completion of treatment must be told this, otherwise, they may not understand why their treatment has been stopped and may try to take treatment from somewhere else. Loss of sensation, muscle weakness and other nerve damage may also remain. Educate the patient about the difference between persistence of light-coloured patches or loss of sensation despite successful therapy as an expected outcome, appearance of new lesions or new sensory loss, nerve involvement, ocular involvement or other signs and symptoms of reaction as danger signs for which the person should report immediately. Ensure that person with disability knows about “self care” for prevention of disability or it’s worsening. (For self care refer POD) Ask persons with low risk for development of reaction/ disability to report immediately on appearance of any of the signs/ symptoms and people with high risk to come for follow up after three months for first year after completion of treatment and every six months for next two years. Those taking steroid therapy are asked to come after two weeks.
After completion of treatment, a very small number of patients may get new skin patches because of relapse. Refer such PAL to referral center for confirmation of relapse and treatment. 7.3.16 Criteria to restart course of MDT On relapse of disease, MDT is restarted. Relapse must be differentiated from Leprosy Reaction. Drop out cases that discontinued MDT for more than three months in PB and more than six months in MB leprosy regimen, restart treatment as other cases Any new lesion reappears after completion of full course of MDT. Refer the case to identified referral center for confirmation of relapse.
What are the complications of not treating?
Complications of leprosy can include:
- Blindness or glaucoma
- Disfiguration of the face (including permanent swelling, bumps, and lumps)
- Erectile dysfunction and infertility in men
- Kidney failure
- Muscle weakness that leads to claw-like hands or an inability to flex the feet
- Permanent damage to the inside of the nose, which can lead to nosebleeds and a chronic, stuffy nose
- Permanent damage to the peripheral nerves, the nerves outside the brain and spinal cord, including those in your arms, legs and feet.
- Nerve damage can lead to a dangerous loss of feeling. A person with leprosy-related nerve damage may not feel pain when the hands, legs, or feet are cut, burned or otherwise injured.
- Approximately one to two million people worldwide are permanently disabled because of leprosy.
What is National/State Programme?
The programme was started in last year of 1st five year plan. The mile stones of the programme are as follows:
- 1955 - National Leprosy Control Programme (NLCP) launched
- 1983 - National Leprosy Eradication Programme launched
- 1983 - Introduction of Multidrug therapy (MDT) in Phases
- 2005 - Elimination of Leprosy at National Level
- 2012 - Special action plan for 209 high endemic districts in 16 States/UTs
- 2016-Leprosy case Detection Campaign in high endemic Area
- 2017-Sparh Leprosy Campaign
What are its objectives?
- Decentralization of NLEP responsibilities to States/ UTs through State/ District Leprosy Societies.
- Accomplish integration of leprosy services with General Health Care System (GHS) and
- Achieve elimination of leprosy at National level by the end of the Project
- Provide good quality leprosy services,
- Enhance Disability Prevention and Medical Rehabilitation,
- Increase advocacy towards reduction of stigma and stop discrimination and Strengthen-
- Monitoring and supervision.
- To achieve elimination of leprosy at national level by the end of the project
- To accomplish integration of leprosy services with general health services in the 27 low endemic states
- To proceed with integration of services as rapidly as possible in the 8 high endemic states
How to achieve these objectives?
A large number of voluntary organizations have been playing a pioneering role in anti-leprosy work in India. While some of them were engaged in training, education and research, others were also engaged, in case detection, treatment, rehabilitation and control work. A large number were voluntary, while some received grants from governmental organizations and others from international agencies.
10. What are the Strategies?
- To eliminate the following strategy adopted:
- Modified leprosy elimination campaigns ( MLEC): organizing camps for 1 or 2 weeks duration for case detection, treatment and referral
- Special action projects for the elimination of leprosy ( SAPEL): initiative for providing MDT services in special difficult to access areas or to neglected population groups.
- Early detection of leprosy cases
- Intensified health education and public awareness campaigns
- Regular treatment of leprosy cases providing multi- drug therapy( MDT) at fixed centres near the patient
- Disability prevention and medical rehabilitation
- Multi-bacillary leprosy is labeled when there are 6 or more skin patches and/or 2 or more nerves affected. Skin smear is positive.
- Paucibacillary leprosy is labeled when there 5 or less than 5 skin lesions and/or 1 more nerve affected. Skin smear do not show bacilli
- Rifampicin is given once a month. No toxic effects have been reported in the case of monthly administration. The urine may be coloured slightly reddish for a few hours after its intake, this should be explained to the patient while starting MDT.
- Clofazimine is most active when administered daily. The drug is well tolerated and virtually non-toxic in the dosage used for MDT. The drug causes brownish black discoloration and dryness of skin. However, this disappears within few months after stopping treatment. This should be explained to patients starting MDT regimen for MB leprosy.
- Dapsone: This drug is very safe in the dosage used in MDT and side effects are rare. The main side effect is allergic reaction, causing itchy skin rashes and exfoliative dermatitis. Patients known to be allergic to any of the sulpha drugs should not be given dapsone.
What is prevalence and New case detection?
- Prevalence Rate (PR): Number of cases on record at a given point of time per 10000 populations.
- New Cases Detection Rate: Number of new cases detected during the year per 100000 populations.
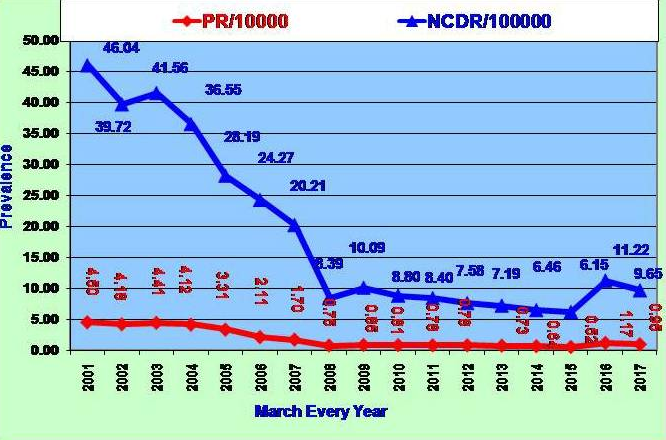
PR and NCDR for last seventeen years.
Migration:
About 54% patients come to Delhi for treatment from neighboring states like UP, Bihar, Haryana Madhya Pradesh and Jharkhand. UP alone contributes almost 28% of new leprosy patients diagnosed in Delhi.

Proportion of mobile patients from neighboring states
What is rehabilitation?
Leprosy may have already permanently damaged the nerves. As they no longer feel pain, a person is then at risk of injuring their hands and feet while completing daily tasks such as walking and cooking. We train people within communities to lead self-care groups which help minimize the risk of injury.
We have specialist shoemakers to build shoes to support a leprosy-affected person’s damaged feet. These have thick soles, often made from old vehicle tyres, so that they cannot be perforated by glass or debris and injure numb feet. Recently more cosmetic MCR footwears are available for better acceptance.
Surgery
The most common leprosy-caused disabilities that can be corrected by surgery are a clawed hand, foot drop and a clawed toe. Movement can be restored by using a muscle transfer technique where, with the help of a physiotherapist, a muscle is identified for transfer and strengthened. After surgery and several weeks in plaster, the patient is taught how to use their old muscle to do a new job and then apply the technique subconsciously. The results can see a leprosy-affected person walk again without dragging their foot on the ground or use their hand to grip items. In a similar way, leprosy patients no longer able to close their eyes as a result of nerve damage (called Lagophthalmos), can undergo Temporalis Muscle Transfer. This sees a muscle used for chewing transferred to the eyes so that, after a period of recovery, a person can close their eyes once again by clenching their teeth. This protects the eyes and can spare a person from blindness.
Prostheses
The fitting of ‘life-like’ prostheses can transform the lives of people who have lost lower legs as a result of leprosy. We offer this opportunity in many of the countries in which we work. A particularly pioneering prosthetic limb service has been launched in Myanmar (Burma). It sees a truck manned by four physiotherapists touring the country making fitting prostheses for leprosy-affected people.
Counseling:
Counseling and tending to the spiritual and emotional needs of people affected by leprosy are an integral part of our care and health services. Counselling is more important than the drug treatment. It’s the heart and soul that matters. The body is temporary, people can overcome physical challenges, but the spirit takes the longest time to heal. For many people the diagnosis of leprosy has taken away all hope. I allow people affected by leprosy to vent their feelings, to cry; emotional healing is so important. Healing is not just medical, it’s a healing of the heart and soul, empowering a person to achieve a life of dignity and worth.”
What services are provided to the affected persons?
- Providing treatment (MDT) to the leprosy affected persons (LEP)
- Deformity correction which are being done in DFIT Goyla Dairy and The Leprosy Mission Hospital (TLM).
- Rupees eight Thousand are being paid to the patients who under goes for the correction of the deformity of Claw hands and drop foot
- To provide MCR footwear.
- Free Medical Services/Medicines are being providing to the LAP and other supported treatment if require.
- Dressing materials are being provided to the LAP having ulcer.
- Weekly visit in the leprosy colonies by NMS/LA/PMW.
- Fortnightly visit in the leprosy colonies by the Medical officer Incharge of the nearby dispensary.
- Monthly visit in the leprosy colonies by the District leprosy officers.
- Budget approved in 2016-17—2.93 Crores
- Budget Proposed 2017-18—3.45 Crores
- What activities are planned this year?
- Quarterly Review Meetings.
- State Level Workshop.
- IEC activities.
- Leprosy case detection campaign (LCDC).
- Chemoprophylaxis are being provided to the contact persons of newly diagnosed LAP
- Focus Leprosy Campaign (FLC) for newly detected grade two disabilities.
- PIP meetings.
- Field level monitoring in leprosy colonies by DLOs.
- Repeat Online reporting system training shall be given to the NMS/LA/MIS experts.
We are How many activities already started?
- Working on IEC activities’
- Planning for quarterly review meeting
What is implementation structure at district level?
At district level NLEP is implemented through district leprosy societies. Each district has a district leprosy officer to implement the programme.
What is reporting system?
Reports are collected in SIS format, compiled and sent to government of India. The system for sending Online Reports to the Central leprosy Division on regular basis is under process. In this regards, the leprosy portal are being started on district level after the training to MIS expert and DLOs of the districts by the ICMR trainers.
How frequently reports are collected and sent to the government?
Monthly, Quarterly and annual reports are being collected from eleven districts, compiled and sent to state and Government of India.
What is the roll of International, National and Local NGOs?
International Federation of anti-leprosy Associations (ILEP) is providing technical support from time to time. ILEP agencies are also helping in reconstructive surgeries and provision of microcellular rubber footwear. They are also conducting sensitization programme for hospital and district administrators.
Involvement of peripheral workers:
Monthly refresher trainings are being imparted to the ASHAs in dispensaries of districts in which a session about the leprosy shall be included.
ASHA is involved in following areas:
- Generating awareness in the community in local language to reduce stigma.
- Encourage self reporting of suspected patients for early case detection and treatment.
- Identify / suspect leprosy completions in the community and refer them to the treatment centre.
- Ensuring leprosy treatment regularity and its timely completion.
- Encouraging leprosy disabled persons to practice self care (as advised by doctor / health worker).
- Encouraging the leprosy affected persons for healthy contact examination of their family.
- AWW worker shall be trained for LCDC activity to be held in 2017.
An urban leprosy project in collaboration with Hind Kusht Nivaran Sangh is being implemented under Bangkok declaration to fill the gaps NLEP. Initially three districts (east, Shahdara and northeast) are selected to improve early case detection, completion of treatment through retrieval of treatment defaulters and prevention of further worsening of disabilities.
For further information /suggestions write to:
Addl. Director/State Leprosy Officer
Govt. of NCT of Delhi
DGHS, Pt DCSS Bhawan, Sector-20
Dwarka- New Delhi-110077
Email: dghsleprosy[at]gmail[dot]com
NATIONAL PROGRAMME FOR PREVENTION AND CONTROL OF DEAFNESS - DELHI
Hearing loss is the most common sensory deficit in humans today. As per WHO estimates in India, there are approximately 63 million people, who are suffering from significant auditory impairment; this places the estimated prevalence at 6.3% in Indian population. As per NSSO survey, currently there are 291 persons per one lakh population who are suffering from severe to profound hearing loss (NSSO, 2001). Of these, a large percentage is children between the ages of 0 to 14 years. With such a large number of hearing impaired young Indians, it amounts to a severe loss of productivity, both physical and economic. An even larger percentage of our population suffers from milder degrees of hearing loss and unilateral (one sided) hearing loss.
OBJECTIVES OF THE PROGRAMME
- To prevent the avoidable hearing loss on account of disease or injury.
- Early identification, diagnosis and treatment of ear problems responsible for hearing loss and deafness.
- To medically rehabilitate persons of all age groups, suffering with deafness.
- To strengthen the existing inter-sectoral linkages for continuity of the rehabilitation programme, for persons with deafness.
- To develop institutional capacity for ear care services by providing support for equipment and material and training personnel.
- To make the public aware about injuries and ear diseases that cause severe or profound hearing loss through IEC activities
STRATEGIES
- To strengthen the service delivery including rehabilitation.
- To develop human resource for ear care.
- To promote outreach activities and public awareness through appropriate and effective IEC strategies with special emphasis on prevention of deafness.
- To develop institutional capacity of the district hospitals, community health centers and primary health centers, selected under the project.
- During 2010-11 the project will be implemented in all the nine districts of Delhi involving major/district hospitals.
ACTIVITIES PROPOSED UNDER PIP:
Availability of man power, procurement of equipment capacity building and required budget proposed in financial year 2010-11 are as follows:-
1. Contractual services: The contractual staff will be engaged under NPPCD to carryout the job effectively.
| Sl. No. | Name of the Post | No. of Posts at State Level | No. of Posts at District/Hospital |
|---|---|---|---|
| 1 | Consultant. NPPCD | 1 | |
| 2 | Audiological assistant | 18 | |
| 3 | Instructor for young Hearing impaired | 18 | |
| 4 | Data Entry Operator | 1 |
The list of the hospitals where services of Audiological assistant and Instructor for young Hearing impaired will be utilized is placed at annexure A. All medical colleges already having specialized facilities will be involved in the programme.
2. Services through ASHA/USHA: ASHAs/USHAs will be involved in diagnosis and follow up of hearing impaired people.
3. Programme Management: State and district programme officers need adequate support for implementation of NPPCD in the state. The support for consumables may be provided to smoothly run the programme.
4.Capacity Building. The training of health care personnel will be conducted as follows:
- 2 days training ENT surgeons /Gynaecologists/ Paediatricians
- 2 Day training to MO PHC/Hosp
- Two day Refresher Training to Audiological Assistant/Instructor
- 1 day Refresher Training PP
- 1 day Refresher Training to Paramedical staff /ANM
- 1 day Refresher Training to School teachers,
- 1 day Refresher Training to ASHA, AWW
5. Behaviour Change Communication: The state and district societies will carry out BCC activities in the state. The meeting with NGOs, Mahila Mandals, community leaders and ASHAs will be organised. Screening camps will be organised in cooperation with NGOs. The funding support should be provided from NRHM
6. Mobility: State and district programme officers may be provided adequate support for mobility for better implementation of NPPCD in the state. The provision for hiring of vehicle is proposed under the programme.
7. Strengthening of hospitals: Following Hospitals will be strengthened with equipment and sound proof rooms under National Programme for Prevention and Control of Deafness (NPPCD).
| District | Name of the Hospital |
|---|---|
| East | 1.LalBahadurShastriHospitalKhichripur, Delhi-91 |
| 2. Dr Hedgewar Arogya Sansthan Karkardooma, Delhi-32 | |
| 4. Chacha Nehru Bal Chikitsalya, Geeta Colony, Delhi-33 | |
| Northeast | 3.JagParveshChandraHospitalShastriPark,Delhi |
| North | 5. Aruna Asaf Ali Hospital Rajpur Road, Delhi-54 |
| Northwest | 6.SanjayGandhiMemorialHospitalMangol Puri,Delhi |
| 7. Bhagwan mahavirhospital Pitampura, New Delhi-34 | |
| 8.BabuJagjeevanRamMemorialHospitalJahangirpuri,Delhi | |
| 9.BabaSahibAmbedkarHospitalSector-6, Rohini New Delhi-85 | |
| 10.MaharishiBalmikiHospitalPooth Khurd,Delhi | |
| 11. Satyawadi Raja Harish Chander hospital Narela,Delhi | |
| West | 12. Deen DayalUpadhyayHospitalHari Nagar, New Delhi-64 |
| 13.GuruGobindSinghGovtHospitalRaghubir Nagar,Delhi | |
| 14.AcharyaSriBhikshuGovtHospitalMoti Nagar, Delhi-15 | |
| Southwest | 15.RaoTulaRamMemorialHospitalJaffarpur, Delhi-71 |
| South | 16.PanditMadanMohanMalviyaHospitalMalviya Nagar New Delhi-17 |
| New Delhi | 17.CharakPalikaHospitalMoti Bagh, New Delhi-21 |
| Central | 18. Dr N C Joshi Hospital Karol Bagh New Delhi-08 |
One hospital in each district will be provided support for sound proof room.
Hospitals under Medical Colleges
- UCMS Guru Teg Bahadur Hospital, Dilshad Garden, Delhi-95
- MAMC Lok Nayak Hospital, JLN Marg, New Delhi-02
- VMMC Safdarjung Hospital, Ring Road,New Delhi
- AIIMS All India Institute of Medical Sciences, Ansari Nagar, New Delhi-29
- LHMC Smt. Sucheta Kriplani and Kalawati Saran Hospitals,New Delhi-01
- PGIMER Dr Ram Manohar Lohiya Hospital, BKS Marg, New Delhi-01
- ACMS Base Hospital, Delhi Cantonment, Delhi-10
8. Equipment: One hospital in each district will be provided sound proof rooms and essential equipment. The PUHCs will be provided PHC Kit and Hearing Aids. The support for Patient welfare will also be provided to the districts to take care of needy patients.
9. Monitoring, supervision Review meeting and workshop: State level workshop and State level quarterly meeting will be conducted to monitor the programme. The required registers and formats will be printed and circulated to the health care units involved in the programme.
The programme is expected to generate the following benefits in the short as well as in the long run.
- Large scale direct benefit of various services like prevention, early identification, treatment, referral, rehabilitation etc. for hearing impairment and deafness as the primary health center / community health centers / district hospitals largely cater to their need.
- Decrease in the magnitude of hearing impaired persons.
- Decrease in the severity/ extent of ear morbidity or hearing impairment in large number of cases.
- Improved service network for the persons with ear morbidity/hearing impairment in the states and districts covered under the project.
- Awareness creation among the health workers/grass root level workers through the primary health centre medical officers and district officers which will percolate to the lowest level as the lower level health workers function within the community.
- Larger community participation to prevent hearing loss through panchyati raj institutions, mahila mandals, village bodies and also creation of a collective responsibility framework in the broad spectrum of the society.
- Leadership building in the primary health centre medical officers to help.
- State of the art department of ENT at the medical colleges in the state/union territory under the project
10. Budgetary Provisions:
An amount of Rs.17171000/- (Rupees One Crore Seventy One Lakhs Seventy One Thousand Only) have been approved during 2010-11 to implement NPPCD in Delhi.
For further Information write/contact to:
State Programme Officer (NPPCD)
Govt. of NCT of Delhi,
Directorate of Health Services
F-17, Karkardooma, Delhi-32
Ph. 011-22304362
Email: baghotia[at]yahoo[dot]com
June 2010
Silicosis Control Programme: Delhi
Introduction:
Silicon Dioxide or Crystallized Silica causes fine levels of dust to be deposited in the lungs. The lungs react in several ways. They get inflamed, create lesions, and then form nodules and fibroids. There are no perceivable symptoms for a numbers of years. Silicosis is difficult to diagnose at its onset. Silicosis symptoms in varying degrees of severity begin to occur. Those affected may experience shortness of breath, fever, chest pain, exhaustion and dry cough. More advanced forms of the disease will show cyanotic mucus membranes and asthma or other breathing difficulties, similar to advanced emphysema. The Silicosis disease may also leave the lung more vulnerable to tuberculosis, and has also been linked to the development of autoimmune disorder such as lupus and rheumatoid arthritis. Since silicosis affects the lungs, it can also affect the vessels leading to the heart. So heart disease and enlargement are common. In the 1990s silicon dioxide was classified as a known carcinogen, and as such. Silica exposure is now linked to the development of lung cancer.
Computerized axial tomography scans and X-rays recognize the lesions and nodules associated with silicosis. Diagnosis is also aided by examining the symptoms of those who may be exposed to silicon dioxide. It is an irreversible condition which can only be addressed by treating the symptoms. Such treatments may include cough syrups, bronchodilators, antibiotics and anti-tubercular medications. Additionally, those affected are advised to avoid exposures to smoking, to any further silica and to other lung irritants. Special filters for drilling equipment have been developed and dry mining is infrequent. Anything that can reduce the silica dust content in the air, particularly the use of water, is employed to make working conditions safer. Precautions developed because of the liabilities for employers, as well as the risk to workers silica exposure lawsuits abound. When the west first began to industries, silicosis contraction was almost certainly if one was employed as a miner or bricklayers. Currently, awareness and government regulations are resulting in fewer new cases of silicosis. Unfortunately; many newly industrialized countries skimp on the cost of prevention at the expense of their workers. These countries will expectedly see a rise in contraction of silicosis until they implement the guidelines protecting their workers. Silicosis will often develop between 20 to 45 years after the exposure. But certain forms of the disease can occur after a single heavy dose to a very high concentration of silica in a short period of time. Workers with Silicosis may have following symptoms:
- Shortness of breath following physical excretion.
- Severe and chronic cough.
- Fatigue, loss of appetite,
- Chest pains and fevers.
Silica particles end up the air sacs of the lung, causing inflammation and scarring that damages the sacs, preventing gas exchange and normal breathing. The disease will be fatal as the inflammation spreads and lung tissue becomes damaged.
Objectives:
- Reduction of new cases of Silicosis in Delhi.
- Capacity building of health care personnel
- Strengthening of diagnostic facilities in health care institutions
- Awareness generation in the community through IEC/BCC activities specially silicosis prone area.
- Clinical care and rehabilitation of silicosis affected people in collaboration with social welfare and urban development department
Strategies:
- Reduction of new cases of Silicosis in Delhi adopting engineering measures specially PPE and keeping fly dust wet.
- Capacity building of health care personnel through trainings, seminars, workshop and advocacy meetings
- Strengthening of diagnostic facilities in health care institutions
- Awareness generation in the community through IEC/BCC activities specially silicosis prone area.
- Clinical care of people affected with silicosis
- Rehabilitation of silicosis affected people in collaboration with social welfare, urban development department and involvement of NGOs
There are three main types detailed below:
- Acute Silicosis: - Occurs after heavy exposure to high concentrations of silica. The symptoms can develop with in a few weeks and as long as five years after the exposure.
- Chronic Silicosis: - Occurs after long term exposure of low concentration of silica dust. This is most common form of the disease and is undetected for many years because a chest X-Ray often does not reveal the disease for a long as 20 years after exposure. This type of the disease severely hinders the ability of the body to fight infections because of the damage to the lungs, making the person more susceptible to other lung diseases including tuberculosis.
- Accelerated Silicosis: - Occurs after the exposure to high concentrations of silica. The disease develops with in 5 to 10 years after exposure. In all three types, silica dust can kill people and can cause many serious diseases besides silicosis. Silicosis can lead to other dangerous lung diseases.
The progression of the Silicosis:
Once in the lungs, the particles cause acute toxicity and damage to the lung cells. Scientists believe that the surface and sharp structure of the silica particles are to blame for the extreme danger and toxic nature of the dust. It has been observed that freshly crushed silica particles cause more inflammation and kill more cells than silica that has in the air. The silica particles are quickly attacked and ingested by the body’s defense system releasing enzymes and radicals. This release of these byproducts can result in death of the lung and white blood cells which causes inflammation and can result in acute silicosis.
As scar tissue is created, it will from lesions in the later stages of the disease. As the body develops chronic inflammation, dark areas becomes visible in X-Ray. The Silicosis nodules are dense spherical structures which collect together and become visible on chest X-rays usually in the upper lung fields. As Silicosis develops the lungs become increasingly susceptible to infection with tuberculosis, fungi and bacteria of many kinds.
The changes in Lungs as Silicosis Progresses:
Acute Silicosis: Acute silicosis is caused by a massive outpouring of protein debris and fluid into lung sacs due to short term exposure to extremely high concentration of silica dust. Acute silicosis is treated with a high dose of steroids, but the prognosis is generally poor. This is because the ongoing accumulation of debris in the lungs air spaces causing respiratory failure which is largely untreatable. Additionally, acute silicosis reportedly has caused many deaths among workers exposed at the same time, at a single work site. Lung Transplants for young workers with this form of silicosis provides some hope.
Chronic Silicosis: In this form of Silicosis, also called chronic nodular silicosis the silicosis nodules collect to form a mass, which can be identified on chest X-ray. These masses cause the upper lobes of the lungs to contract, which appears as an “angel wing pattern” on the X-rays. Doctors and radiographers refer to this pattern as angel of death because it is a poor prognostic sign.
Accelerated Silicosis: Accelerated Silicosis is a very rare form that progresses rapidly from intense short term exposure to silica particles. In this form, the nodules develop at a much faster rate and are usually fatal within a few years.
Prevention of other complications of the disease:
- Infections:- Fungal infections are believed to result when the lung scavenger cells that fight these disease are overwhelmed with silica dust and are unable to kill mycobacterium .
- Silico tuberculosis: - Patients with silicosis have a greatly increased risk of developing tuberculosis.
- Systematic Sclerosis: - Silica exposure has been associated with systemic sclerosis and its many forms. Systemic sclerosis is a disorder of connective tissues and joints and small blood vessels. Scleroderma involves skin changes and injury to the joints and small blood vessels. Sclerosis involves skin changes and injury to the joints changes are seen on the skin, particularly over the fingers and face.
- Silica Associated Lung Cancer: - Lung cancer has been associated with preexisting silicosis. However, lung cancer may also occur in person exposed to silica in the absence of silicosis. Doctors believe that silicosis produces increased risk for lung cancer and that the association between silica exposure and lung cancer is causal.
Silicosis Diagnosis & Treatment:
Workers have been overexposed to silica dust should visit a doctors specializing in lung disease, a pulmonologist. Silicosis often goes untreated and undiagnosed especially chronic silicosis because its symptoms are not unique. A person’s occupational history with silica dust exposure will help doctors evaluate possible medical problems. Through medical examination using chest X-rays and lung function test can determine if a person has silicosis. Workers at risk of exposure, such as miners or sandblasting should have lung examination at least every 3 years. Above all, prevention of the disease is key action to control silicosis, because there is no way to reverse the disease. Lung function tests are useful in early diagnosis of the disease, often showing poor airways and bronchitis associated with irritation from the dust.
Using tools like CT Scans, MRIs, invasive procedures are almost never required to make the diagnosis of silicosis as a simple Chest X-ray is a good tool. Patients at risk should let their doctor know, because the doctor may not think to look for the disease. There are risks of misdiagnosis. It may be misdiagnosed as pulmonary edema and Tuberculosis. Few lasting treatment are available for silicosis. The first step is obviously stopping continuing exposure. This will not stop the gradual progression the disease, but will prevent it form an even faster rate of progression.
Treatment aim to relieve pain and suffering: Patients are administered oxygen and steroids to help them breathe as the disease runs its course. Unfortunately the only good treatment for end-stage silicosis is a lung transplant, which can be a lifesaving treatment.
The General Control of the Disease:
- Use of Oxygen
- Patients stops smoking
- Monitoring the person for signs of lung infection
- Experts have also tried aluminum powder, d-pencillamine., and polyvinyl pyridine-N-Oxide.
Govt. Effort for Silicosis Control in Lal Kuan Area:-
Lal Kuan is a small urban village near the Mehrauli-Badarpur Road. It has been an active mining and quarrying area with a large numbers of stone crushers that have helped in building of Delhi. All the crushing and mining operations came to a halt in 1992 by Supreme Court Order. This judgment, though reduced the pollution level of Delhi, its ambiguous position on the issue of occupational health hazards made the lives of the poor workers more vulnerable. When mining crushing activities were on, everything in Lal Kuan used to be covered by a thick layer of dust. Most of the victims are migrant workers. Both husband and wife are suffering from silicosis/others respiratory problems in majority of households.
Today, Lal Kuan is the home of former mine workers and stone crushers ailing from silicosis. Prasar (An NGO) claims that at least 3, 000 residents have died in the last 15 years from silicosis tuberculosis and other breathing ailments in Lal Kuan area. NGO must be having some records or Gastimates only? But it is sensitive to the problem of silicosis in poor population. Chief Minister Delhi convened a meeting in Delhi Secretariat to discuss the problem of silicosis in the Lal Kuan area,. The meeting was attended by the Health Minister of Govt. of Delhi, Food Minister, Principal Secretary (Health & Family Welfare), Directors Social welfare, and Director Health Services (DHS) and other officers of different departments. Representatives of NGO-Prasar along with the silicosis victims were also present to explain the sufferings of silicosis victims in Delhi. Chief Minister asked the officials to find long term rehabilitation for the silicosis victims. The medical examination and physical survey of the area was advised to provide benefits to needy population.
Physical Survey:
Physical survey was the joint venture of directorate of social welfare and directorate of health services. The team consisted of 1) District Social Welfare Officer, 2) Research Officer, DHS, 3) Kanungo, Revenue Department 4) CDPO of Area 5) NGO-PRASAR, 6) Anganwadi workers (AWWs) involved=17. The Social welfare Departments has carried out its physical survey to bring the silicosis victims into Antyodaya schemes and granting of pensions.
Strengthening of Services
Health department is generating awareness about silicosis in the community. Doctors are being sensitized to suspect and detect cases of silicosis. The media interest on occupational hazards has triggered the voice to review occupational safety rules and implement them strongly across the country. The most significant effect has been on the minds of the inhabitants of Lal Kuan. It has driven away the feeling of hopelessness and instilled sense of empowerment among the people giving them a new zeal to look forward to life. Active involvement of NGOs has brought public private partnership.
Mobile medical vans are now visiting for four days a week. It is distributing free medicines for silicosis and other respiratory and Occupational diseases. The building of the Hospital/PUHC at Tajpur with X-ray facility needed for the detection of the silicosis is almost complete. The survey of the medical team is complete a short report on the health survey has also been submitted to the Delhi Government.
Medical Survey:-
The health survey results show that, about 68 percent of the symptomatic people surveyed suffer form silicosis, silico-tuberculosis. A large percentage of people also suffer from hearing loss and malnutrition. The survey stressed on the need for continued surveillance of the health of the people and a further comprehensive study on the health of Lal Kuan victims.
Clinical Examination:
The Dean MAMC constituted a task force comprising Dr. T.K Joshi from COEH, Dr. K.S. Baghotia of DHS, and Dr. Neeraj Gupta of COEH. Two surveyors were appointed who were trained and provided guidance in feeling up the interview schedules. The chest X-ray Blood & Urine investigations were required for the subjects under study were carried out at NTPC Hospital Badarpur. The radiographer as per norms were read by:- Dr Arthur Frank, chief of occupational health, Drexel University, Philadelphia. Dr. Rahul Mukherjee, MRCP, a Respiratory Physician in Birmingham Hospital U.K and Dr T.K. Joshi, Occupational Physician of COEH trained in UK and USA. Pulmonary function testing was performed by Dr. Neeraj Gupta of COEH.
Findings:
Out of 240 cases suspected to be symptomatic only 165 symptomatic subjects presented for the study and 111 turned up for X-ray. Out of this only 104 subjects had occupational history. Almost 98 subjects presented with a history of working in stone crushers. Out of this 41 were found to be having silicosis. Only one case of silicosis did not have exposure. It appears that the exposure to dust was associated with silicosis in about 45% of those who worked on stone crushers. 43% patients were also having deafness. In addition to this 82% subjects had low hemoglobin levels i.e., Anemia.
Validation of Silicosis Cases:
Forty four (44) candidates were identified by the medical team headed by Dr. T.K. Joshi suffering from silicosis/ silico-tuberculosis. An expert group was constituted in MAMC under Prof. M.K. Daga to further examine these patients and provide medical help/health care. Twenty one (21) patients were confirmed by the experts group and validated to be suffering from silicosis/silico-tuberculosis in Delhi. This list has been sent to concerned Commissioner under Workman compensation Act and Chief Inspector Factories for further action and Help to the silicosis victims.
Awareness Activities:
Directorate of health services has conducted outdoor awareness activities involving metro trains and metro railings keeping in view widely distributed construction workers engaged all over Delhi.
Rehabilitation Strategies:
- A medical team consisting of occupational health experts’ conducted clinical survey of the affected person in Lal Kuan area.
- A multi purpose Community Health Centre (CHC) for the treatment of the occupational disease will be built at the Tajpur near Lal Kuan.
- The social welfare department, health department and the urban development department will also explore and provide alternative livelihood opportunities for the citizens of Lal Kuan.
Advisory
For further Information write/contact to:
State Programme Officer (Silicosis)
Govt. of NCT of Delhi,
Directorate of Health Services
F-17, Karkardooma, Delhi-32
Ph. 011-22304362
Email: baghotia[at]yahoo[dot]com


 स्वास्थ्य सेवा महानिदेशालय
स्वास्थ्य सेवा महानिदेशालय 


